NL|17 – 08 February 2017
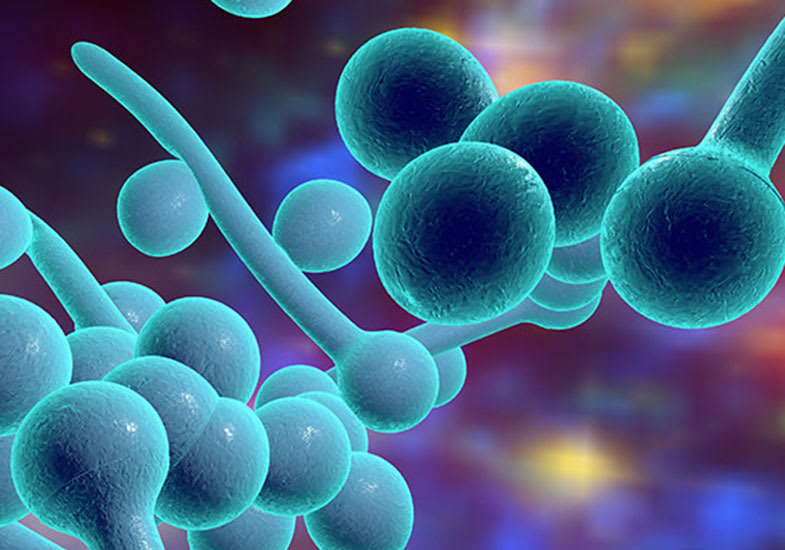
Candidiasis: fungal infection
that affects various parts of the body
Candidiasis (or candidosis) is a fungal infection caused by any type of Candida yeast, a saprophyte fungus belonging to the Saccharomyces family that physiologically lives in the oral cavity, gastrointestinal tract, on skin, in the vagina and in the mucosa of healthy people.
Its excessive growth however may determine the onset of symptoms that vary based on the affected part of the body and hot-humid parts are most at risk as well as areas of skin most prone to sweating and humidity:
- Infection that develops in the mouth or throat is called “thrush” or oropharyngeal candidosis;
- Vaginal infection is often called “yeast infection”;
- Invasive candidosis occurs when fungi penetrate the circulatory system and spread to the entire body.
Vaginal Candidiasis is rather common among women of childbearing age and is not risky but is particularly bothersome and manifests itself in a highly characteristic way, with a classic sensation of itchiness, often associated with a burning sensation and discharge.
Women in childbearing age and who are sexually active
are most at risk. Often this disease may also present itself in infants and newborn babies (nappy rash). Even men can be affected by candidosis, although the disease can present itself in an asymptomatic form.
In physiological conditions, Candida is silent because it presents itself in the form of a spore, adhering to epithelial cells of the vagina without harming them, whereas when virulent, it may assume the active form of hypha.
The infection occurs when adhesion turns into penetration and invasion of the vaginal epithelial lining, through the release of proteolytic enzymes and toxins, with acute inflammation and pain.
The turning point between one form or another depends on a dynamic balance between the aggressive characteristics of the fungus and the host’s active immune-surveillance response.
It is a highly common disturbance which in most cases presents itself several times during the affected person’s lifetime. Almost 75% of women present this type of disease at least once in their life and in 90% of cases it is caused by a fungus called Candida albicans. Of these, around half will present with successive episodes due to recurrent onset. 28.1% of adolescents who seek help at public doctor’s surgeries for a gynaecological visit have Candida vulvovaginitis; 20% of vaginal culture tests of asymptomatic women are positive for Candida; lastly, 20-22% of acute infections evolve to become vulvovaginitis from recurring Candida (Recurrent Vulvo Vaginal Candidiasis, RVVC), characterised by four or more episodes per year.
Candida albicans, as previously mentioned, is the most common form of candida, however mixed infections are on the rise, caused simultaneously by fungi and bacteria, as are infections caused by other species of the same family, for example:
• C. Glabrata, diagnosed in 54% of diabetics compared to 22.6% of non-diabetic women;
• C. Krusei and Tropicalis, more frequent in diabetics;
• C. Parapsilosis and Lusitaniae, rarer compared to others.
The methods of transmission of Candida include:
- Self-infection, especially from intestinal reservoir:
a) due to contamination of vulva skin with residual faecal matter;
b) due to the translocation of Candida inside and through intestinal mucosa cells, especially in cases of colon wall inflammation, irritable bowel syndrome, diverticulosis, ulcerative colitis and so on.
- Sexual transmission
- Maternal-foetal transmission, during birth or vaginally
The intestine-hidden instigator of many forms of vaginal infection- still remains the main source of Candida colonisation in the vagina.
Candida isolated by rectal cultures in patients with RVVC is identical to the one found in the vagina, suggesting the existence of a persistent intestinal reservoir of the fungus, a concept that has been clear since the 70s.
It is important to be aware that in all form of candidiasis and fungal infection there is the concomitant presence of intestinal candida, so as to undertake the right treatment for the patient, with the adoption of precise treatment plans that are also personalised, with both topical and oral products that provide effective action against the etiopathogenetic mechanisms of the disease, aiming for prophylaxis in the event of recurrence, clinical healing and eradication of the pathogen.