NL|08 – 13 May 2016

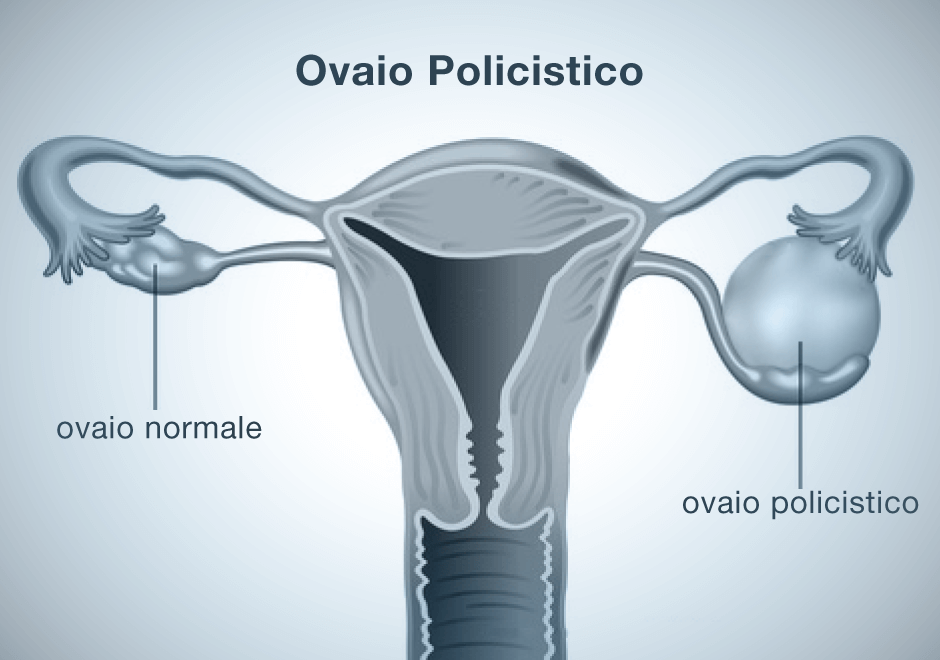
Polycystic ovary syndrome
is frequent in women with type 1 diabetes
Polycystic Ovary Syndrome (Pcos) is frequent in women with type 1 diabetes mellitus and may contribute towards reduced fertility, with a mechanism that does not directly depend on the glycemic and metabolic control of diabetes. This is why screening for the syndrome and high androgen levels should be included in current guidelines for the management of type 1 diabetes in women.
This is a summary of the conclusions of a study published in Diabetes Care, by the main author Hector Escobar-Morreale from the diabetes, obesity and human reproduction work group at the Ramon y Cajal University Hospital in Madrid, Spain. “Some studies carried out on small numbers of cases report an increase in the prevalence of polycystic ovary syndrome and symptoms of excess androgen in women with type-1 diabetes. With the aim of improving knowledge on the association between the syndrome and diabetes, using meta analysis we systematically reviewed the prevalence of polycystic ovary syndrome and hyperandrogenism in adolescent and adult women with type 1 diabetes”, the authors write, after searching studies on the topic in major biomedical archives.
Upon completing the analysis the researchers selected nine trials conducted on 475 adult and adolescent women with type 1 diabetes, discovering that the prevalence of polycystic ovary syndrome and traits associated with hyperandrogenism in women with type 1 diabetes was 24% for polycystic ovary syndrome, 25% for hyperandrogenism and hirsutism, 24% for menstrual dysfunctions and 33% for polycystic ovarian morphology (Pcom), a condition whose symptoms are not necessarily obvious.
“These figures are notably higher than previous ones in the general population without diabetes and considering that polycystic ovary syndrome has substantial negative consequences for the health of women with type 1 diabetes, routine screening for the syndrome and relative traits in such women seems justified, also in order to increase knowledge of the problem and enable the successive preparation of guidelines based on evidence.
Underlying mechanisms of this association remain largely unknown: one possible explanation is that exogenous hyperinsulinism, deriving from the subcutaneous administration of exogenous insulin, may trigger the production of androgens by the ovary in predisposed subjects”, the authors conclude.
Diabetes Care April 2016. doi: 10.2337/dc15-2577